Tunable White LED Lighting Poised to Improve Life in Nursing Homes
 More than anyone else, people in nursing homes struggle to find high-quality sleep, which is especially disheartening because we know that elderly people are more susceptible to health issues, which poor sleep can exacerbate. While this is a complex issue, there is a good deal that we can do about it because we understand how our brains decide when it is time for us to be awake and when it is time for us to be asleep. It comes down to our circadian rhythm, which melatonin regulates. Naturally, it was the absence of the sun that would initiate melatonin production. This is still true, but other variables have come into play.
More than anyone else, people in nursing homes struggle to find high-quality sleep, which is especially disheartening because we know that elderly people are more susceptible to health issues, which poor sleep can exacerbate. While this is a complex issue, there is a good deal that we can do about it because we understand how our brains decide when it is time for us to be awake and when it is time for us to be asleep. It comes down to our circadian rhythm, which melatonin regulates. Naturally, it was the absence of the sun that would initiate melatonin production. This is still true, but other variables have come into play.
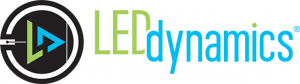
![]() Let’s dive into this a little deeper. When we talk about melatonin production and sleep, we need to talk about the circadian rhythm too. This is what determines how our brain directs our sleeping and waking functions, and while you may be able to fall asleep when you are outside the rhythm, sleep quality will suffer. This is because the hypothalamus inside the brain struggles to operate properly when the circadian rhythm is out of alignment with reality, and when its suprachiasmatic nucleus (SCN) cannot work in conjunction with the optic nerve behind the eye, it receives unclear signals about light and darkness and makes inaccurate conclusions about day and night.
Let’s dive into this a little deeper. When we talk about melatonin production and sleep, we need to talk about the circadian rhythm too. This is what determines how our brain directs our sleeping and waking functions, and while you may be able to fall asleep when you are outside the rhythm, sleep quality will suffer. This is because the hypothalamus inside the brain struggles to operate properly when the circadian rhythm is out of alignment with reality, and when its suprachiasmatic nucleus (SCN) cannot work in conjunction with the optic nerve behind the eye, it receives unclear signals about light and darkness and makes inaccurate conclusions about day and night.
For thousands of years – the vast majority of history, even the majority of some older people’s lives – all of this information would have been interesting but certainly not immediately relevant. If you experienced minimal or no exposure to artificial lighting, how could this information have been relevant? Today, though, we all come into contact with artificial lighting, almost constantly, and at night, that spells trouble for the circadian rhythm. Just when your brain is trying to figure  out when it is time for you to go to sleep and when it is time for you to wake up, you are looking at your phone or your tablet, exposing yourself to blue light, and throwing your circadian rhythm out of sync.
out when it is time for you to go to sleep and when it is time for you to wake up, you are looking at your phone or your tablet, exposing yourself to blue light, and throwing your circadian rhythm out of sync.
For younger, healthier people, it is possible to throw the circadian rhythm out of sync and still fall asleep at night. It is possible in the way that it is possible to eat unhealthy foods for a day without falling ill, but it is not the ideal. In nursing homes, on the other hand, sleep challenges are already widespread. If you have ever visited a nursing home yourself, then you may have observed these challenges in action, the difficulties that many residents face when they are trying to sleep or when they are trying to go about their days and inadvertently falling asleep. As one study out of the University of California put it, “Although older community-dwelling adults are more likely to take naps than younger adults, the typical long-term care resident shows a pattern of wakefulness that is frequently interrupted by brief periods of sleep.”
 When sleep issues already run rampant, any solutions could prove groundbreaking, and in nursing homes, sleep challenges do run rampant. Before the influx of blue light that smart phones and smart pads ushered in, sleep quality was already critical to elderly people because of the health issues that arise from poor sleep. Falling short of their sleep requirements and falling ill or sleeping during the day, during inopportune moments, elderly people may try to make up for sleep that they missed at night, but as research has shown, this concept is false: we cannot make up for sleep once we have missed it. As you surely know yourself if you have ever tried to go through a Monday on only two or three hours of Sunday-night rest, quality of sleep impacts quality of life, but what else does it mean for people? How does a smooth circadian rhythm affect our lives?
When sleep issues already run rampant, any solutions could prove groundbreaking, and in nursing homes, sleep challenges do run rampant. Before the influx of blue light that smart phones and smart pads ushered in, sleep quality was already critical to elderly people because of the health issues that arise from poor sleep. Falling short of their sleep requirements and falling ill or sleeping during the day, during inopportune moments, elderly people may try to make up for sleep that they missed at night, but as research has shown, this concept is false: we cannot make up for sleep once we have missed it. As you surely know yourself if you have ever tried to go through a Monday on only two or three hours of Sunday-night rest, quality of sleep impacts quality of life, but what else does it mean for people? How does a smooth circadian rhythm affect our lives?
Irritability, poor concentration, poor memory, slower reaction times, decreased performance: these are all well-known symptoms of low-quality sleep. In the elderly – in particularly the elderly who suffer from dementia, a condition already associated with the same symptoms – these symptoms can become overwhelming, to the point that research published in Neuropsychiatric Disorders and Treatment concluded that over a ten-year period, there was a link between insomnia and elderly suicide.
Knowing this, we also know that we need to do something to respond to these challenges. The Pandora’s box of blue light is open, and there is no turning back. We can encourage people to avoid their phones in the evening over and over again, but we need something more active to respond to these challenges effectively. To determine how we can respond to these challenges, it is useful to look beyond circadian rhythm and its theoretical effects and consider the real-world effects of circadian rhythm in nursing homes – and how circadian lighting can make a difference.
Circadian Lighting Effects in Nursing Home
To figure out what circadian lighting could mean to nursing homes, we can look to the research. One study from the US Department of Energy is especially encouraging, pointing to the game-changing numbers that they have seen circadian lighting drive and the inimitable impact that this lighting can have on populations where the rates of sleep disturbances are high – as we said, even affecting a majority of all the people within the population.
 In this study, out of the ACC Care Center, researchers consider the residents of the 99-bed facility as a whole. They stated, “The objective was to test a strategy for measuring and documenting light exposure for typical residents, and to evaluate the collected data in terms of multiple metrics for human circadian responses over the course of a day.” This is an important point to make because, as they also point out, this science is still new. Newer than the blue-light-emitting devices that exacerbated these sleep issues in the first place. Dependable tunable white lighting is an innovation that, unfortunately, most nursing home professionals and administrators have not heard of. When we see the undeniable effects of circadian lighting in nursing homes, that is the only explanation that would make any sense, too.
In this study, out of the ACC Care Center, researchers consider the residents of the 99-bed facility as a whole. They stated, “The objective was to test a strategy for measuring and documenting light exposure for typical residents, and to evaluate the collected data in terms of multiple metrics for human circadian responses over the course of a day.” This is an important point to make because, as they also point out, this science is still new. Newer than the blue-light-emitting devices that exacerbated these sleep issues in the first place. Dependable tunable white lighting is an innovation that, unfortunately, most nursing home professionals and administrators have not heard of. When we see the undeniable effects of circadian lighting in nursing homes, that is the only explanation that would make any sense, too.
For their study, researchers for the US Department of Energy depended on three models for circadian wellness, each of which purports to tell us how light is impacting sleep quality: melanopic/photopic (M/P) ratios, equivalent melanopic lux (EML), and circadian stimulus (CS). Let’s consider each of these models.
For an M/P ratio, we are considering the melanopic content and the photopic content, both measured at the eye. Sometimes, experts will refer to this as the “blue-cyan content” because that is what it is describing, the blue light that is at an eye. When the M/P ratio is high, it leads to wakefulness, and when the M/P ratio is low, it leads to sleepiness.
An EML, meanwhile, accounts for the radiant watts that our ipRGC photoreceptors detect and the photopic content at the eye – again, higher equating to more wakefulness and lower equating to more sleepiness.
Then, there is CS, which measures the suppression of melatonin, once again the higher values equating to wakefulness and the lower ones equating to sleepiness.
 The researchers for the ACC Sleep Center study used what we call “spectrophotometers” (Konica-Minolta CL-500a) read the radiant energy data necessary to calculate M/P ratio, EML, and CS, detecting light in the nursing home environment so that they could compare their readings to the objective reports that the nursing home residents submitted regarding their sleep quality. From this, we can extrapolate calculations and objective reports into conclusions about the effects of different types of lighting on elderly people’s sleep quality.
The researchers for the ACC Sleep Center study used what we call “spectrophotometers” (Konica-Minolta CL-500a) read the radiant energy data necessary to calculate M/P ratio, EML, and CS, detecting light in the nursing home environment so that they could compare their readings to the objective reports that the nursing home residents submitted regarding their sleep quality. From this, we can extrapolate calculations and objective reports into conclusions about the effects of different types of lighting on elderly people’s sleep quality.
Making a point of controlling the static lighting at 4100K, the researchers strove to imitate the eye lighting conditions in the morning for all residents so that they could say more definitively that they were observing results caused through nighttime lighting conditions. This means that when we are reviewing the statistics and conclusions in this study, we can say with a high degree of confidence that we are reviewing the effects of nighttime lighting conditions as well.
The researchers also worked from an assumption that has become mostly universal by now among those who are familiar with the different types of lighting and their effects: low, warm-color light leads to stronger melatonin production, which leads to higher sleep quality. Pictures were taken of the same corridor, but at different times of the day to provide a visual example of the tuning range (Photo from Report is Below).

Time and again, the outcome was clear: tuned white lighting made a difference. Anything but indecisive, their research showed a significant gap between the sleep disturbances that residents experienced when exposed to old styles of lighting and the sleep disturbances their counterparts experienced when exposed to cutting- edge tuned white lighting. Static lighting, repeatedly, correlated with higher incidences of sleep disturbances in this nursing home.
edge tuned white lighting. Static lighting, repeatedly, correlated with higher incidences of sleep disturbances in this nursing home.
It is important to realize that the static lighting the researchers used was no different from the static lighting that nearly all nursing homes are using at this very moment. The environments that they replicated for their study would have been indistinguishable from many other real-world nursing home environments, which begs the question: how many elderly people are suffering needlessly? How many people in nursing homes are laying awake at night, unable to get their circadian rhythms in balance, unable to fix their melatonin production, falling asleep in the middle of the next day when their families are visiting them? What are the repercussions of sleep disturbance in regards to the nursing staff?
The gap between static lighting and tuned white lighting, it turns out, is a chasm. You may be wondering, How serious could the difference have been? As far as science goes, the answer is very. Exposed to tuned white lighting, residents experienced only half as many sleep disturbances as they would have exposed to static lighting – 1.8 versus 3.6. In research of this kind, that is the type of determinative difference that researchers are looking for, either to confirm their hypothesis or deny it. When only half as many nursing home residents are experiencing sleep disturbances while exposed to some stimulus, that stimulus merits further attention, to say the least.
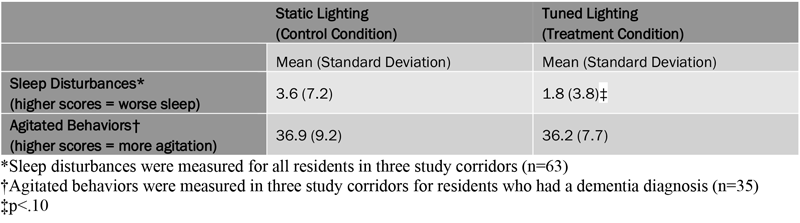
Researchers were even more direct in their conclusions about the study, stating that “The intervention likely worked to reduce sleep disturbances in the 5% to 7% of residents with many severe sleep disturbances.” While 5% to 7% is a minority of all residents, it would be difficult to overstate how life-altering it could be to reduce their severe sleep disturbances because, again, these challenges result in more than irritability and poor concentration. Over time, severe sleep disturbances, like insomnia, can lead to a number of irreversible health issues, up to and including suicide.
The researchers, reviewing their M/P ratio, EML, and CS calculations, determined that tunable white lighting was effective at cutting down on blue-cyan content at night and at delivering higher levels of blue-cyan content in the morning and during the day, when wakefulness becomes important. In every way, this lighting seemed capable of improving quality of life at the ACC Care Center, calculation after calculation turning out positive and in favor of the newer lighting type.
Astoundingly, the researchers for the US Department of Energy also reported that “[I]n an institutional setting with shared rooms, such as the nursing center in this study, improving the sleep of a few residents may have a ripple effect on roommates and closely located others.” Put another way, we can create a wave of health benefits by improving nursing home residents’ sleep, thinking beyond the immediate and measurable figures that we are examining in M/P ratio, EML, and CS calculations. It is rational to assume, therefore, that in a nursing home, everyone benefits from tuned white lighting.
Lighting to Improve Life
 Tunable white lighting – often referred to, appropriately, as circadian lighting – has shown promise as a sleep aid in a way that no other innovation has. When we think of the defining role that smart devices are playing in our lives, their smorgasbords of blue light filling us up and damaging our melatonin production whether we like it or not, this means that tunable white lighting could be the answer. This could be the technology that we all need to reclaim higher-quality sleep for ourselves and make a pointed shift away from the low-quality sleep that would come to define this era otherwise.
Tunable white lighting – often referred to, appropriately, as circadian lighting – has shown promise as a sleep aid in a way that no other innovation has. When we think of the defining role that smart devices are playing in our lives, their smorgasbords of blue light filling us up and damaging our melatonin production whether we like it or not, this means that tunable white lighting could be the answer. This could be the technology that we all need to reclaim higher-quality sleep for ourselves and make a pointed shift away from the low-quality sleep that would come to define this era otherwise.
In nursing homes, the concerns that we are raising rise beyond the level of convenience and desire. Because of the high rates of insomnia and sleep disturbances that already permeate these environments, we need solutions now. These are pressing circumstances, and if we ignore them, we are setting ourselves up for disaster. Likewise, if we respond to these circumstances effectively, we can do incredible things – even saving lives. There is an opportunity to make life better for people, showing our friends and family in nursing homes that we care and that we are willing to take steps to show that.
Circadian lighting, or white tuned lighting, is the next frontier in lighting, and it seems right that nursing homes would find themselves pioneering into it. Blue-cyan content, shaping wakefulness and sleepiness the way that it does, ought to come back under the control of the professionals and caregivers who think of nursing homes as their calling. For the residents who depend on them, this innovation could mean the difference between one life and another – between high-quality sleep and something else.
The statistics are clear. Today, nearly half of all adults age 60 and up report insomnia, and more than half report some form of sleep disturbance. For those who think of insomnia and sleep disturbances as natural byproducts of age, we would point to the facts that the US Department of Energy and other researchers have uncovered in their studies. Better is possible, achievable through modest interventions. Something as straightforward as changing out some lighting can slash sleep disturbance rates in half, returning  elderly people to sleep habits and circadian rhythms that are truly natural, correcting the flaws that blue-light saturation has introduced.
elderly people to sleep habits and circadian rhythms that are truly natural, correcting the flaws that blue-light saturation has introduced.
PERFEKTLIGHT is our answer to all of the questions and demands that this research has presented. We have engineered our tuned white lighting system with the human body’s circadian rhythm at the forefronts of our minds. Because we are so enthusiastic about the difference that this innovative lighting can make, we have devoted ourselves to perfecting it. Our system not only draws on the benefits of tuned white lighting in general but also enhances and optimizes the technology, taking it to a whole new level.